This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box is welcome.
Case presentation:
A19 year old boy presented with pain abdomen since morning of 25th september
HOPI : patient was apparently asymptomatic 1week back then he had 2 glasses of toddy and chicken on last Friday. After 2 days(on Sunday)he developed pain for the first time and had 1 episode of vomiting .He also had nausea.No H/O constipation,distension,jaundice ,diarrhoea.
The pain spontaneously reduced for few days which is sudden onset,pricking type,proggesive in nature, aggrevated on sleeping on same side and on standing ,subsides on its own in 1 hour
It is associated with vomiting which is non bilious with food contents and non foul smelling
No H/O back ache,pain In loin , groin,mass per abdomen
No H/O fever, weight loss,night sweats,dyspnea,chest pain.
The patient complaint of feeling of fullness and belching immediately after meals and pricing type of pain in right upper quadrant after meals
PAST HISTORY: known case of Asthma 4 years ago and taken medication,used for 2-3months and then stopped medication.
Diagnosed with anemia 4 years back and used iron supplements.
No H/O HTN,DM,epilepsy,TB,CAD
FAMILY HISTORY :No H/O similar complaints inthe family
PERSONAL HISTORY:
He was on mixed diet, appetite normal, bowel habits normal and occasionally toddy drinker
GENERAL EXAMINATION: pt is conscious, coherent, cooperative and oriented to time, place and person mildpallor
no Icterus,cyanosis,clubbing, lymphadenopathy,edema
VITALS:
Temperature-99.8°f on presentation
BP:140/90mmhg
PULSE:79pm
RR:19cpm
Spo2:98%
GRBS:103mg/dl
PER ABDOMEN:
INSPECTION : Abdomen bilaterally symmetrical.
No distention of abdomen,no flank fullness.
All quadrants moving equally with respiration.
Umbilicus is central and inverted.
Cupid bow sign present
No scars,sinuses,striae,pigmentation,echymosis,dilated veins and visible pulsations.
PALPATION: No Guarding and rigidity.
Diffuse tenderness present more in left iliac region
No palpable liver ,spleen
Kidney is ballotable.
All hernial orifices are free.
No sister joseph nodule present.
PERCUSSION : No fluid thrill.no shifting dullness
AUSCULTATION : Bowel sounds not present.
CVS:s1 s2 heard
RS: BAE clear, normal vesicular breath sounds heard,no added sounds
CNS: Higher mental function normal
Cranial nerves intact
Motor system: intact
Sensory system: intact
INVESTIGATIONS :
Chest X-Ray

ECG

Serum amylase

RFT

LFT

Lipase

Hemogram

BUN

CUE

USG
Treatment :
1) NPO till further orders
2)IV fluids NS -1unit - 125ml/hr
3) RL -1unit. -125ml /hr
4) DN -1unit - 125mlhr
5) Inj pan 40 mg IV OD
6) Inj Tramadol in 100ml NS IV BD
7) In zofer IV SOS
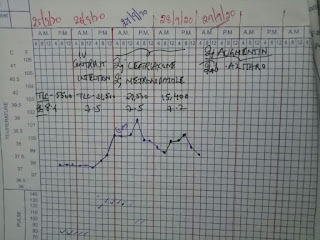
8)Bp,pulse,temperature,spo2 charting
9)GRBS charting
10)I/O strict monitoring
11) Abdominal girth daily
Day 1. On 26th sep at 8:00am
No fresh complaints
O/E : patient is conscious,coherent and cooperative
Vitals : patient is afebrile
BP : 140/90 mmHg
PR : 83bpm
P/A : soft,diffuse tenderness present in left iliac fossa
CVS : S1S2 heard
R/S : Bilateral air entry present
CNS : Normal
INVESTIGATIONS : serum ferritin
CECT
2D ECHO
Treatment :1)NPO till further orders
2)IV fluids NS - 2units- 125ml/hr
3) RL. -2units -125ml /hr
4) DNS -2units - 125mlhr
5) Inj pan 40 mg IV OD
6) Inj Tramadol in 100ml NS IV BD
7) In zofer IV SOS
8)Bp,pulse,temperature,spo2 charting
9)GRBS charting
10)I/O strict monitoring
11) Abdominal girth daily
On 26th sep at 3:30pm :
He complained of chills after post contrast after 10 mins
Then gradually developed tachycardia around 150-160 bpm
He was given phenaramine and hydrocortisone
His chills were decreased temporarily but tachycardia doesnt
Then gradually his bp fall around 80/10
On vigorous treatment with iv fluids and noradrenaline infusion systolic bp is maintained around 110 but diastolic still ranging around 20-40 mmhg and als he complained of unable to pass urine though bladder was full and can be palpable suprapubically on examination he has congenital phimosis
On passing feeding tube around 850 ml of urine was drained
And also to decrease histaminic symptoms im phenargine was given
INVESTIGATIONS :
ECG at 8pm :

ECG at 9pm :
2D ECHO :
At 5pm His IVC was 1.6/1.2cm
At 9pm :
At 2:30am : IVC was 1.7 to 2.2 cms
RFT :-
ABG :-
Day 2 :- 27th sep
No fresh complaints
O/E : patient is conscious,coherent and cooperative
Pallor present ,
Noicterus,clubbing,cyanosis,
lyphmadenopathy,oedema
BP : 100/10mmg Hg
PR : 130bpm
RR : 29c/m
GRBS : 131mg/dl
Spo2 : 97% on room air
I /O :3600/1450ml
Abdominal girth : 74cms
P/A : soft, non tender
Cvs : s1s2 heard
R/S : Bilateral air entry present
INVESTIGATIONS :
Hemogram
RFT
ABG
Chest X -ray
Serology :
HIV,HBsAg,HCV - negative
Treatment:
1) NPO till further orders
2)IV fluids NS@2units - 125ml/hr
3) RL@2units -125ml /hr
4) DNS @2units- 125mlhr
5) Inj pan 40 mg IV OD
6) Inj Tramadol in 100ml NS
7) In zofer IV SOS
8)Bp,pulse,temperature,spo2 charting
9)GRBS charting
10)I/O strict monitoring
11) Abdominal girth daily
12) Temperature monitoring 2nd hourly
13) Inj Normal if temp is ≥ 101°F
14) Tepid sponging
15) Inj Cetriaxone 1gm IV/BD
16 ) Inj Metrogyl 100ml/IV/TID
17) Inj Hydrocort 100mg/IV/TID
Day 3 : sep 28th :-
C/O 3 episodes of brown coloured loose stools(resolved)
O / E : patient is conscious,coherent and cooperative
Vitals : pt is febrile
Bp : 130/60 mmg Hg(koratkoff 4)
PR : 110bpm ,regular
RR : 22c/m
GRBS : 117mg /dl
Spo2 :98%on room air
Abdominal girth : 72cms
I/O : 3000 / 1950ml
There is pallor ,mild icterus,facial puffiness,right upper limb oedema.
P/A : soft non tender
CVS : s1s2heard
R/S : Bilateral air entry present
CNS : Normal
INVESTIGATIONS :
Hemogram
RFT
LFT
CUE
Stool for occult blood
2D-ECHO
Treatment :
Treatment : 1) Inj Cetriaxone 1gm /Iv/ BD
2)IV fluids NS - 125ml/hr
3) RL. -125ml /hr
4) DN - 125mlhr
5) Inj pan 40 mg IV OD
6) Inj Tramadol in 100ml NS IV BD
7) In zofer IV SOS
8)Bp,pulse,temperature,spo2 charting
9)GRBS charting
10)I/O strict monitoring
11) Abdominal girth daily
12) Inj Metrogyl 100ml/IV/TID
13)) Inj Hydrocort 100mg /IV/BD
Day 4: sep 29th :-
No fresh complaints
O/E : patient is c/c/c
Vitals : Bp : 120/50 mm hg
PR : 120bpm
RR : 22c/m
Spo2 : 96%
GRBS : 138mg/dl
I / O : 3250/1800 ml
Pallor present ,facial puffiness subsiding
2-3 rashes seen over forearm
CVS : s1s2 heard
Rs : clear ,less breath sounds in right intra axillary area
INVESTIGATIONS :
Hemogram :
Treatment :
1) Ini AUGMENTIN 1.2g IV BD
2)Tab Azithromycin 500mg po /OD
3) soft diet (low in fat and high I'm early digestible carbohydrates)
4) oral fluids 1.5L / day
5) Inj pan 40 mg IV OD
6) Inj Tramadol in 100ml NS IV BD
7) In zofer IV SOS
8)Bp,pulse,temperature,spo2 charting
9)GRBS charting
10)I/O strict monitoring
11) Abdominal girth daily
12) Inj Neomol if temp ≥ 201° f
13)) Inj Hydrocort 100mg /IV/BD
Day 5 : sep 30th
No fresh complaints
O/E : pt is c/c/c
Vitals :pt is afebrile
Bp : 130 /80mmhg
PR : 108bpm
RR : 30c/m
GRBS : 187mg /dl
Spo2 : 98%on room air
AG : 84cms
I/O : 3250/1800
Jvp raised
Cvs : s1s2 heard
Rs : bilateral air entry present
INVESTIGATIONS :
Hemogram
Treatment :
1) Ini AUGMENTIN 1.2g IV BD
2)Tab Azithromycin 500mg po /OD
3) soft diet (low in fat and high I'm early digestible carbohydrates)
4) oral fluids 1.5L / day
5) Inj pan 40 mg IV OD
6) Inj Tramadol in 100ml NS IV BD
7) In zofer IV SOS
8)Bp,pulse,temperature,spo2 charting
9)GRBS charting
10)I/O strict monitoring
11) Abdominal girth daily
12) Inj Neomol if temp ≥ 201° f
13)) Inj Hydrocort 100mg /IV/BD
Day 6 :oct 1st
No fresh complaints
O/E : pt is c/c/c
Vitals :pt is afebrile
Bp : 120/60mmhg
PR : 96bpm
RR : 22c/m
GRBS : 99mg /dl
Spo2 : 98%on room air
AG : 84cms
I/O : 1900 /1000
Jvp raised
Cvs : s1s2 heard
Rs : bilateral air entry present
INVESTIGATIONS :
2d echo
USG
Stool for culture and sensitivity
Blood for culture and sensitivity
Treatment :
1) Ini AUGMENTIN 1.2g IV BD
2)Tab Azithromycin 500mg po /OD
3) soft diet (low in fat and high I'm early digestible carbohydrates)
4) oral fluids 1.5L / day
5) Inj pan 40 mg IV OD
6) Inj Tramadol in 100ml NS IV BD
7) In zofer IV SOS
8)Bp,pulse,temperature,spo2 charting
9)GRBS charting
10)I/O strict monitoring
11) Abdominal girth daily
12) Inj Neomol if temp ≥ 201° f
Diagnosis :- Acute pancreatitis with gross Ascites with Anaphylactoid reaction after
Contrast injection.